"Order alli 60 mg amex, weight loss while breastfeeding".
By: J. Dawson, M.B.A., M.D.
Clinical Director, Northwestern University Feinberg School of Medicine
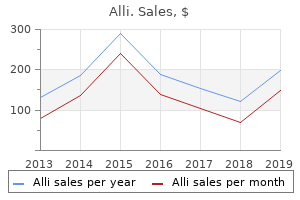
Specifically weight loss 5 pounds buy cheap alli 60 mg online, improvements in sound localization and speech understanding have been noted weight loss pills and cleanse discount alli 60mg with amex. Bilateral implantation can be staged months apart or undertaken safely in one setting When a second implant is placed weight loss oils order alli 60mg line, monopolar cautery must be avoided. There are a myriad of variables that can be adjusted to improve the sound quality. After the first day, most adults report that speech sounds like static or voices sound either like "Donald Duck" or sound metallic in character. Amazingly, without any changes to the device, over the next 24 hours the sound quality improves. This learning by the brain occurs mostly within the first 36 months, after which the rate of improvement in sound quality slows. Most adults have programming sessions 46 times in the first year, then annually or as needed. Children (particularly infants) are more difficult to program because of the lack of a consistent feedback response regarding volume and clarity. Objective intraoperative measurements are helpful in estimating hearing thresholds and comfort levels. Programming is critical to the success of the device, and experienced audiologists are able to achieve better outcomes than less experienced audiologists. The anticipation of an abnormal nerve location and the use of intraoperative facial nerve monitoring should result in very few cases of temporary or permanent nerve injury. Tinnitus Patients need to understand that the residual hearing in the ear with the implant is likely to be lost and that a hearing aid will be of no benefit. Cochlear trauma from device insertion not only results in a loss of hearing, but it also may lead to or exacerbate tinnitus. When encountered in this setting, tinnitus typically lessens in time and often markedly improves after device programming. Vestibular Dysfunction Breaching the confines of the inner ear may also result in vestibular dysfunction with temporary balance problems; however, permanent balance difficulty has, in rare cases, been reported as well. Electronic Malfunction Although the implanted device has no moving parts to wear out, there are still instances of electronic malfunction or failure due to trauma. In particular, risks such as those encountered when removing a cholesteatoma or performing any surgery for chronic ear pathology do exist, including wound infection, facial nerve injury, taste disturbance, tinnitus, and balance problems. Overall, the complication rate of cochlear implantation has been reported as being 510%. Risk of Meningitis the risk of meningitis in implant recipients is being scrutinized. Patients with inner ear malformations have a higher risk of meningitis pre- and postoperatively unrelated to the cochlear implantation. The role of the electrode design and its impact on the risk of meningitis is under investigation. It is prudent for adult and pediatric implant recipients to receive the available pneumococcal vaccine; moreover, children should be vaccinated against Haemophilus. Wound Infection A postoperative wound infection can usually be adequately treated with local wound care and antibiotics, but because of the presence of an indwelling foreign body, explantation of the device is occasionally required. Wound or skin breakdown can occur with an acute infection or may be related to excessive pressure of the magnet over the implant. It is important for patients to monitor the condition of the skin between the magnet and the implant device; the magnet strength can be adjusted to account for skin thickness. Adult implant recipients with positive outcomes have seen benefits as far-reaching as a restored capability to communicate on the telephone (attained by roughly 60% of adult recipients) and the ability to converse without the necessity of lip-reading. Other selected benefits that have been described include the treatment of tinnitus, the improvement of preimplantation depression, and a perceived overall improvement in the quality of life (reported to be as high as 96% of recipients in one report). Rarely in medicine is there a procedure that has such a profoundly positive impact on the quality of life.
When the pressure in the ear canal corresponds with the pressure in the middle ear cavity weight loss excess skin best purchase for alli, the tympanic membrane is at its most compliant point and thus absorbs weight loss vegetarian diet order alli 60 mg visa, rather than reflects weight loss pills in pakistan order generic alli from india, the most sound. The tympanometric peak, or maximum flow of acoustic energy into the middle ear, occurs when the pressure in the ear canal and middle ear is equal. If the middle ear is not properly aerated, the middle ear pressure will be negative (> 100 daPa). Thus, the ear canal 601 pressure corresponding to the tympanometric peak provides an estimate of middle ear pressure. For infants and neonates, tympanograms obtained using a 226Hz probe tone may appear normal erroneously; therefore, a higher-frequency probe tone (660 or 1000 Hz) must be used. Classification Traditionally, tympanograms have been classified as Type A, Type B, or Type C (Figure 454). Some clinicians prefer describing the tympanogram in a more specific narrative form. The volume measurement that is simultaneously performed with tympanometry helps to differentiate between a flat tympanogram suggesting an intact eardrum with middle ear effusion and a perforated eardrum or patent ventilating tube. Acoustic reflex thresholds refer to the softest intensity levels that can trigger the response. When the muscle contracts, the stapes footplate rocks in the oval window and stiffens the ossicular chain and tympanic membrane, thus decreasing compliance. The change in compliance coincident with the presentation of an intense acoustic signal is measured with the same instrument as that used for tympanometry. Because monaural stimulation results in contraction of the stapedius muscles in both ears, the reflex can be measured either ipsilaterally or contralaterally. When the reflex is recorded in the stimulated ear, it is called an ipsilateral reflex; if it is recorded in the opposite ear, it is called a contralateral reflex. Knowledge of this pathway allows the clinician to compare the results of the various testing configurations to interpret the findings. Patients with mild or moderate cochlear (sensory) hearing loss yield contralateral and ipsilateral acoustic reflex thresholds at approximately the same intensity levels as those with normal hearing. Acoustic reflexes are absent in the presence of a severe or profound hearing loss. A significant conductive hearing loss typically eliminates the response on either ear whenever the affected side is stimulated. This is because the stimulating sound is not loud enough to trigger the reflex when the affected ear is stimulated, and the middle ear abnormality (eg, otosclerosis or middle ear effusion) prevents the stapedius muscle from contracting even when the opposite (normal) ear is stimulated. Therefore, any disorder of the stapedius muscle can also cause absent acoustic reflexes. Thus, the only reflex that will occur for a unilateral conductive loss is the ipsilateral reflex to the normal ear. However, contralateral and ipsilateral reflexes are usually present when the normal ear is stimulated. For pathologies affecting the central crossed pathways, reflexes are present in both ipsilateral conditions, but may be absent in the two contralateral conditions. A lesion of the seventh nerve (eg, Bell palsy) can eliminate the acoustic reflex whenever the affected side is measured, regardless of which ear is stimulated. This pattern can be distinguished from the conductive pattern because in a conductive loss, both the measured and the stimulated ear typically show absent contralateral reflexes. In seventh nerve pathology, the acoustic reflex also can help to determine whether the lesion is proximal or distal to the branching of the stapedius muscle. If the lesion is proximal to the stapedius muscle, acoustic reflexes are absent; if the lesion is distal to the muscle, reflexes are present. A functional hearing loss may be suspected if reflexes occur below the volunteered puretone thresholds or possibly (though not always) if less than 20 dB above threshold. Usually, acoustic reflex decay is only measured contralaterally at 500 or 1000 Hz, because higher frequencies and ipsilateral stimulation may show decay even in normal subjects. Also, care must be taken in deciding whether or not to administer decay testing, especially in patients with tinnitus or hyperacusis, because of the intense stimulus levels that are often required. The obtained results can be extrapolated to provide information regarding hearing sensitivity and also can be used for neurodiagnostic purposes.
Complications of tracheotomy include bleeding weight loss pills expired cheap alli 60mg mastercard, infection weight loss exercise program generic 60mg alli with amex, crusting or mucus plugging weight loss pills endorsed by dr oz buy generic alli line, pneumothorax, and accidental dislodgment of the tracheotomy tube. Late postoperative complications include tracheoesophageal fistula, tracheal stenosis, tracheocutaneous fistula, and airway stenosis. Perioperative Care and General Otolaryngology 21 Percutaneous Dilation Tracheotomy A percutaneous dilation tracheotomy is not to be used in an emergent airway situation: this procedure is only to be performed on patients who are already intubated. There are several different techniques all widely based on the Seldinger technique (needle and catheter over guide wire). Relative contraindications include poor neck landmarks, morbid obesity, previous neck surgery, limited neck extension, and severe coagulopathy that is not correctable. At least two persons are needed: one to perform the tracheotomy, the other to manage the endotracheal tube and video bronchoscope. An incision is made either horizontally or vertically between the cricoid and the suprasternal notch and an introducer needle is placed into the trachea at about the second ring; this is confirmed with bubbling of air and with simultaneous video bronchoscopy. In addition, transillumination of light from the bronchoscope can be used to help demarcate the best site for the introducer needle. A J-tipped guide wire is then placed under direct visualization through the catheter into the trachea. Again, every step should be bronchoscopically visualized on the video monitor during the procedure. This is removed and once dilation of the anterior tracheal wall has been performed, a percutaneous tracheotomy appliance is placed over the guide wire and positioned in the airway. Following this, the bronchoscope should be withdrawn from the endotracheal tube and introduced via the tracheotomy tube to confirm placement in the airway. It is then secured using four sutures on all corners of the flange and a tracheotomy tie is also used to secure the appliance around the neck. A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Therefore, valuable information may be obtained by the use of various radiographic techniques. Other imaging modalities, such as angiography, are used for specific conditions such as vascular lesions. Perioperative Care and General Otolaryngology 23 neck, laryngeal structures, facial bones, and temporal bone. The incoming radiation is continuously registered and the signal is digitized and fed into a data matrix taking into account the varying beam angulations. Multidetector scanners have several rows of photoreceptors, allowing the simultaneous acquisition of several slices. Helical techniques allow patients to move continuously through the scanner instead of stopping for each slice. These advances have significantly decreased scan times and radiation exposure while improving spatial resolution. Newer in-office flat plate cone beam scanners can rapidly acquire 1-mm slice thickness images of the sinus and temporal bone with very low radiation exposure. A rotating curved detector field opposite to the tube registers the attenuated fan beam after it has passed through the patient. Taking into account the tube position at each time point of measurement, the resulting attenuation values are fed into a data matrix and further computed to create an image. This is done by placing the patient in a strong magnetic field, which initially aligns the hydrogen nuclei in similar directions. High-resolution ultrasound is used for head and 26 Handbook of OtolaryngologyHead and Neck Surgery neck anomalies such as thyroglossal duct cysts, branchial cleft cyst, cystic hygromas, salivary gland masses, abscesses, carotid body and vascular tumors, and thyroid masses. Working Principle of Ultrasound An alternating electric current is sent through piezoelectric crystals; it vibrates with the frequency of the current, producing sound waves of that frequency. Ultrasound gel acoustically couples the ultrasound transducer to the body, where the ultrasound waves can then spread.
The pia mater is adherent to weight loss pills cvs proven 60 mg alli the spinal cord weight loss with hypothyroidism cheap alli online american express, and the posterior longitudinal ligament is attached to weight loss 30 10 weight loss for life proven 60mg alli the posterior aspect of the vertebral bodies. The subdural space is only a potential space between the dura and arachnoid mater. General somatic afferent fibers are conveyed from the skin of the back via the dorsal primary rami. Communicating rami contain general visceral efferent (sympathetic) fibers and general visceral afferent fibers of the autonomic nervous system. Ventral primary rami convey mixed spinal nerves to/from all other parts of the body excluding the back, and parts of the head innervated by cranial nerves. The conus medullaris is located at the L1-2 vertebral level; therefore, any choice that contains that region is the correct answer. L3-4 is a common location to perform lumbar puncture, but it is caudal to the apex of the conus medullaris. Meningitis is an inflammation of the meninges caused by bacteria, viral, or numerous other irritants. It does not cause deformation of vertebrae or result in protrusion of spinal cord contents. Spina bifida occulta is a normally asymptomatic condition in which the vertebral lamina fail to fuse completely during embryologic development. A tuft of hair is commonly seen growing over the affected region (usually lumbar in position). Somatic afferent fibers convey localized pain, typically from the body wall and limbs. Sympathetic preganglionic fibers are visceral efferent fibers and do not contain sensory information. Parasympathetic preganglionic fibers are also visceral efferents and do not contain sensory information. Lateral flexion is the best answer because other movements of the lumbar portion of the vertebral column are very limited due to the orientation of the articular facets. The acromion (the highest point of the shoulder) is the part of the scapula that forms the "point" of the shoulder. The glenoid of the scapula articulates with the head of the humerus to form the glenohumeral joint. The spine of the scapula is located posteriorly and separates supraspinous and infraspinous fossae. This includes the C7 spinal nerve because it exits the vertebral column above the C7 vertebra. The trapezius would be intact because it is innervated by the spinal accessory nerve. The deltoid muscles and supraspinatus muscles will be unaffected because they receive motor supply from C5 and C6. The rhomboid muscles should function normally because they are innervated by the dorsal scapular nerve (C5). The latissimus dorsi muscles would not function normally because they are innervated by the thoracodorsal nerves, which receive contributions especially from the C7 spinal nerves. Spina bifida cystica refers to spina bifida with meningocele and is the correct answer. Cranium bifida could present with meningocele in the skull, but it would not be located in the lower back. Spina bifida occulta is a defect in the formation of the vertebral arches and does not present with meningocele. Hemothorax refers to blood accumulation in the pleural space surrounding the lungs. ArnoldChiari malformation is a herniation of the medulla oblongata and cerebellum through the foramen magnum and would not present with pathologies in the lower back. The lumbar triangle (of Petit) is bordered medially by the latissimus dorsi, laterally by the external abdominal oblique, and inferiorly by the iliac crest. An indirect inguinal hernia is located in the inguinal canal of the anterior abdominal wall. A direct inguinal hernia is located in the Hesselbach triangle of the anterior abdominal wall.
There is more consensus that percutaneous tracheotomy is best avoided in children (higher complication rate weight loss pills qatar buy alli 60mg fast delivery, difficulty ventilating with a bronchoscope through the ventilating tube) weight loss pills vicky discount 60 mg alli with mastercard. Excluding children weight loss xtreme buy discount alli, current literature supports endoscopic percutaneous tracheotomy as a viable alternative to surgical tracheotomy if performed by an experienced surgeon. Early Infection Hemorrhage Subcutaneous emphysema Pneumomediastinum Pneumothorax Tracheoesophageal fistula Recurrent laryngeal nerve injury Tube displacement Delayed Tracheal-innominate artery fistula Tracheal stenosis Delayed tracheoesophageal fistula Tracheocutaneous fistula 521 C. Suctioning the tube and trachea on a frequent basis immediately postoperatively is necessary to clear secretions and prevent plugging. The frequency of suctioning can be decreased as the postoperative time increases and the patient recovers. Also, changing the tracheotomy tube can usually be performed at this time, after an adequate tract has formed. Patency can be evaluated either with a mirror exam of the larynx or by direct fiberoptic endoscopy. The patient with an adequate airway after tube occlusion should tolerate decannulation; tube removal is usually performed after 24 hours of tube occlusion. Occasionally, subcutaneous emphysema results when air is trapped in the subcutaneous tissues from suturing the surgical incision. The physician must monitor for the potential development of either pneumomediastinum or pneumothorax if the condition progresses. Pneumomediastinum results when air is sucked through the wound or from coughing that forces air into the deep tissue planes of the neck and into the mediastinum. Pneumothorax may result from progressive pneumomediastinum or from direct injury to the pleura during tracheotomy. A tracheoesophageal fistula can occur if the tracheal incision is made too deep, causing inadvertent injury to the underlying esophagus. Recurrent laryngeal nerve damage is possible if dissection occurs lateral to the trachea. Tube displacement is a risk of surgery and can be minimized by the use of stay sutures or the Bjцrk flap. One of the most dire complications of tracheotomy is a tracheal-innominate artery fistula, which occurs when the major vessel is eroded by pressure necrosis from the tracheotomy cuff or directly from the tip of the tube itself. It usually presents within 2 weeks of the tracheotomy and carries a 73% mortality rate. The treatment consists of controlling the hemorrhage by overinflating the tracheotomy tube cuff or inserting an endotracheal tube below the level of bleeding while compressing the innominate artery anteriorly against the sternum, with the index finger inserted through the tracheotomy wound. Tracheal stenosis is another delayed complication and can occur at the level of the stoma, the tracheotomy tube cuff, or the tube tip. A tracheoesophageal fistula can also occur in the delayed setting and is considered to be secondary to pressure necrosis from the tracheotomy tube cuff or the tip of a malpositioned tube. An indwelling nasogastric tube may predispose the patient to postoperative complications. A persistent tracheocutaneous fistula can sometimes occur after decannulation of a long-standing tracheotomy. Closure involves excising the fistula tract and closing, in layers, the trachea, strap muscles, platysma, and skin. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Endoscopic percutaneous dilatational tracheotomy: a prospective evaluation of 500 consecutive cases. The Consumer Products Safety Act was passed in 1979 and includes criteria for the minimum size of objects (> 3. Children older than 5 years have been found to be more likely to aspirate school supplies than food. Children with esophageal motility disorders or neurologic disorders should be encouraged to chew food slowly and completely to avoid esophageal impactions or aspiration. Clinical Findings General Considerations Foreign body ingestions are an important cause of morbidity and mortality in the pediatric population. Aerodigestive tract foreign bodies are the cause of approximately 150 pediatric deaths per year in the United States, and choking causes 40% of accidental deaths in children less than 1 year of age. A high level of clinical suspicion can prevent delays in diagnosis and complications related to these delays. Information that is important to elicit from parents includes the approximate time of ingestion, any history of esophageal dysfunction, and both the severity and the duration of swallowing and respiratory symptoms since the time of ingestion.
Order alli without a prescription. Weight Loss Yoga Day 4 Challenge! Fat Burning 20 Minute Workout Beginners & Intermediate.