"Discount anafranil 75 mg line, bipolar depression and relationships".
By: M. Mannig, M.B. B.CH. B.A.O., Ph.D.
Deputy Director, New York University Long Island School of Medicine
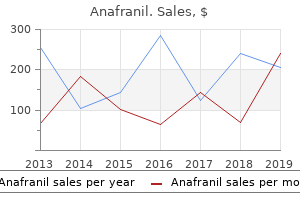
It rarely appears in the vertical plane alone anxiety games anafranil 10 mg generic, suggesting then a tegmental brainstem disorder or lithium intoxication depression test by doctors anafranil 10 mg for sale. Oscillopsia is the illusory movement of the environment in which stationary objects seem to great depression definition dictionary buy cheapest anafranil and anafranil move back and forth, up and down, or from side to side. With lesions of the labyrinths (as in aminoglycoside toxicity), oscillopsia is characteristically provoked by motion-. Downbeat nystagmus, which is always of central origin, is characteristic of lesions in the medullary-cervical region such as syringobulbia, Chiari malformation, basilar invagination, and demyelinative plaques. It has also been seen with Wernicke disease and may be an initial sign of either paraneoplastic brainstem encephalitis or cerebellar degeneration with opsoclonus. Downbeat nystagmus, usually in association with oscillopsia, has also been observed in patients with lithium intoxication or with profound magnesium depletion (Saul and Selhorst). Halmagyi and coworkers, who studied 62 patients with downbeat nystagmus, found that in half of them this abnormality was associated with the Chiari malformation and various forms of cerebellar degeneration; in most of the remainder, the cause could not be determined. However, a large proportion of cases of downbeating nystagmus remain unexplained by any of these mechanisms. Nystagmus of several types- including gaze-evoked nystagmus, downbeat nystagmus, and "rebound nystagmus" (gazeevoked nystagmus that changes direction with refixation to the primary position)- occurs with cerebellar disease (more specifically with lesions of the vestibulocerebellum) or with brainstem lesions that involve the nucleus prepositus hypoglossi and the medial vestibular nucleus (see above, in relation to upbeat nystagmus). Characteristic of cerebellar disease are several closely related disorders of saccadic movement (opsoclonus, flutter, dysmetria) described below. Tumors situated in the cerebellopontine angle may cause a coarse bilateral horizontal nystagmus, coarser to the side of the lesion. Nystagmus that occurs only in the abducting eye is referred to as dissociated nystagmus and is a common sign of internuclear ophthalmoplegia, as discussed above. Pendular Nystagmus this is found in a variety of conditions in which central vision is lost early in life, such as albinism and various other diseases of the retina and refractive media (congenital ocular nystagmus). Occasionally it is observed as a congenital abnormality, even without poor vision. The defect is postulated to be an instability of smooth pursuit or gaze-holding mechanisms. It is purely or mainly pendular (sinusoidal) except in extremes of gaze, when it comes to resemble jerk nystagmus. The oscillations of the eyes are usually very rapid, increase on upward gaze, and may be associated with compensatory oscillations of the head and intolerance of light. Indications as to the congenital nature of nystagmus are that it remains horizontal in all directions of gaze; it is suppressed during convergence and may be associated with odd head positions or with head oscillations and with strabismus. Also characteristic is a paradoxical response to optokinetic testing (see below), in which the quick phase is in the same direction as the drum rotation. A related latent nystagmus is the result of a lack of normal development of stereoscopic vision and may be detected by noting that the nystagmus changes direction when the eyes are alternately covered. In addition, severe visual loss or blindness of acquired type that eliminates the ability to accurately direct gaze, even in adulthood, produces nystagmus of pendular or jerk variety. Both horizontal and vertical components are evident and the characteristic feature is a fluctuation over several seconds of observation in the dominant direction of beating. Spasmus mutans, a specific type of pendular nystagmus of infancy, is accompanied by head nodding and occasionally by wry positions of the neck. Most cases begin between the fourth and twelfth months of life, never after the third year. The nystagmus may be horizontal, vertical, or rotatory; it is usually more pronounced in one eye than the other (or limited to one eye) and can be intensified by immobilizing or straightening the head. Most cases are idiopathic, but symptoms like those of spasmus mutans betray the presence of a chiasmal or third ventricular tumor (see also seesaw nystagmus below). The explanation of this phenomenon is that the slow component of the nystagmus represents an involuntary pursuit movement to the limit of comfortable conjugate gaze; the eyes then make a quick saccadic movement in the opposite direction in order to fixate a new target that is entering the visual field. These observations indicate that an abnormal response does not depend on a lesion of the geniculocalcarine tract. Presumably the loss of the pursuit phase with a parietal lesion is due to interruption of efferent pathways from the parietal cortex to the brainstem centers for conjugate gaze. On the other hand, frontal lobe lesions allow the eyes to tonically follow in the direction of the target but with little or no fast-phase correction in the direction opposite the lesion.
Accessible rapid-acting carbohydrates and frequent blood glucose monitoring before depression test hpb best buy anafranil, during depression psychiatric definition purchase anafranil on line amex, and after exercise depression recurrence symptoms purchase 75mg anafranil mastercard, with or without continuous glucose monitoring, maximize safety with exercise. Consider additional carbohydrate intake during and/or after exercise, depending on the duration and intensity of physical activity, to prevent hypoglycemia. For low- to moderate-intensity aerobic activities (30260 min), and if the patient is fasting, 10215 g of carbohydrate may prevent hypoglycemia (17). In addition, obesity is as common in children and adolescents with type 1 diabetes as in those without diabetes. It is associated with higher frequency of cardiovascular risk factors, and it disproportionately affects racial/ethnic minorities in the U. Therefore, diabetes care providers should monitor weight status and encourage a healthy diet, exercise, and healthy weight as key components of pediatric type 1 diabetes care. B Rapid and dynamic cognitive, developmental, and emotional changes occur during childhood, adolescence, and emerging adulthood. Early detection of depression, anxiety, eating disorders, and learning disabilities can facilitate effective treatment options and help minimize adverse effects on diabetes management and disease outcomes (33,35). Furthermore, the complexities of diabetes management require ongoing parental involvement in care throughout childhood with developmentally appropriate family teamwork between the growing child/teen and parent in order to maintain adherence and to prevent deterioration in glycemic control (36,37). As diabetes-specific family conflict is related to poorer adherence and glycemic control, it is appropriate to inquire about such conflict during visits and to either help to negotiate a plan for resolution or refer to an appropriate mental health specialist (38). Monitoring of social adjustment (peer relationships) and school performance can facilitate both well-being and academic achievement (39). Suboptimal glycemic control is a risk factor for underperformance at school and increased absenteeism (40). Shared decision making with youth regarding the adoption of regimen components and self-management behaviors can improve diabetes self-efficacy, adherence, and metabolic outcomes (22,41). E Mental health professionals should be considered integral members of the pediatric diabetes multidisciplinary team. E Encourage developmentally appropriate family involvement in diabetes management tasks for children and adolescents, recognizing that premature transfer of diabetes care to the child can result in diabetes burn-out nonadherence and deterioration in glycemic control. A Providers should consider asking youth and their parents about social adjustment (peer relationships) and school performance to determine whether further intervention is needed. B Offer adolescents time by themselves with their care provider(s) starting at age 12 years, or when developmentally appropriate. E Starting at puberty, preconception counseling should be incorporated into routine diabetes care. Beginning at the onset of puberty or at diagnosis of diabetes, all adolescent girls and women with childbearing potential should receive education about the risks of malformations associated with poor metabolic control and the use of effective contraception to prevent unplanned pregnancy. Preconception counseling using developmentally appropriate educational tools enables adolescent girls to make well-informed decisions (43). Youth with type 1 diabetes have an increased risk of disordered eating behavior as well as clinical eating disorders with serious short-term and longterm negative effects on diabetes outcomes and health in general. With respect to disordered eating, it is important to recognize the unique and dangerous disordered eating behavior of insulin omission for weight control in type 1 diabetes (50). The presence of a mental health professional on pediatric multidisciplinary teams highlights the importance of attending to the psychosocial issues of diabetes. These psychosocial factors are significantly related to self-management difficulties, suboptimal glycemic control, reduced quality of life, and higher rates of acute and chronic diabetes complications. E Please refer to Section 7 "Diabetes Technology" for more information on the use of blood glucose meters, continuous glucose monitors, and insulin pumps. More information on insulin injection technique can be found in Section 9 "Pharmacologic Approaches to Glycemic Treatment," p. Current standards for diabetes management reflect the need to lower glucose as safely as possible. When establishing individualized glycemic targets, special consideration should be given to the risk of hypoglycemia in young children (aged,6 years) who are often unable to recognize, articulate, and/or manage hypoglycemia. However, registry data indicate that lower A1C can be achieved in children, including those,6 years, without increased risk of severe hypoglycemia (51,52). Type 1 diabetes can be associated with adverse effects on cognition during childhood and adolescence.
Buy 75 mg anafranil with visa. 11 bipolar celebrities you had no idea about.
Restraints may be required but should be used sparingly given that patients who struggle against them may undergo worse rhabdomyolysis (Lahmeyer and Stock 1983) depression youtube order 25mg anafranil with amex. Agitation anxiety breathing exercises anafranil 75 mg free shipping, delusions bipolar depression symptoms quiz purchase anafranil overnight, and hallucinations, if problematic, may be treated with an antipsychotic such as haloperidol (Giannini et al. Dystonia, if severe, and opisthotonus may be treated with intravenous lorazepam, and seizures may be treated with intravenous lorazepam and, if repetitive, fosphenytoin. Vigorous general medical care may be required for hyperthermia, hypertension, and rhabdomyolysis. The treatment of the various post-intoxication sequelae is discussed in the respective sections on these syndromes. Once intoxication and any post-intoxication sequelae have resolved, efforts should be undertaken to ensure abstinence, which may include involvement in Narcotics Anonymous. Course Occasional recreational use of either phencyclidine or ketamine, without consequences, is not uncommon in late adolescence or early adult years. Prolonged and repeated use, despite medical or social consequences, appears uncommon, and such abuse of these drugs tends to resolve while patients are still in their twenties. The full panoply of these is often seen in alcoholism, and this disorder is also discussed. Differential diagnosis Hallucinogen intoxication resembles mild intoxication with phencyclidine or ketamine, although it lacks some of p 21. In moderate intoxication, the behavior becomes coarse and the thinking is slow and unclear. There is facial flushing, conjunctival injection, dysarthria, nystagmus, and ataxia. With severe intoxication there is drowsiness, stupor, and disabling ataxia; coma may ensue, with respiratory depression and death. In an alcohol-naive subject, mild intoxication is seen at 100 mg%, moderate intoxication at 200 mg%, and severe intoxication at 300 mg%; in the alcohol-naive patient, levels of 400 mg% generally cause coma, and levels of approximately 500 mg%, respiratory depression. Of interest, females tend to become intoxicated with a smaller amount of ingested alcohol than males, and this may be because of a reduction in gastric alcohol dehydrogenase activity, thus allowing a greater percentage of the ingested alcohol to escape this initial metabolic step (Frezza et al. This is characterized by headache, malaise, dysphoria, nausea, mild tremulousness, and diaphoresis. If, however, short-term memory is tested during the blackout, one finds that patients are unable to recall anything that happened much more than 5 minutes earlier. Should blacked-out patients fall asleep during the blackout, they may, upon awakening the next day, anxiously ask acquaintances what they did the night before. Those who are still awake when the blackout abruptly ends may be quite startled at their situation; one patient (Goodwin et al. Pathological intoxication (Perr 1986), although long written of (Banay 1944; May and Ebaugh 1953), is a controversial diagnosis (Coid 1979). Putatively, patients, after only a small amount of alcohol, undergo a dramatic change, becoming uncharacteristically irritable and often violent. One study was able to reproduce these symptoms in patients thought to have suffered pathologic intoxication (Maletzky 1976), whereas another was not (Bachy-Rita et al. Tolerance to alcohol typically develops gradually with chronic, repeated intoxications, and greater and greater amounts must be drunk to achieve the desired intoxication. In such cases, patients who had previously been able to consume a liter of liquor and still be standing may now find themselves hopelessly and severely intoxicated after only a few drinks. Symptoms include tremulousness, anxiety, easy startability, poor memory and concentration, fleeting and poorly formed visual or auditory hallucinations, insomnia (Johnson et al. The most prominent symptom of alcohol withdrawal, however, is tremor, and it is from this that the syndrome derives its colloquial name. The tremor is postural, rapid, and ranges in amplitude from fine to coarse; it may be confined to the outstretched hands or be more widespread, even generalized, involving the eyelids and tongue in severe cases. This does offer temporary relief of the shakes but of course threatens to set off a vicious cycle. Alcohol withdrawal generally peaks within a couple of days and then gradually settles over the next 2 or 3 days.
In one study mood disorder hotline buy anafranil online from canada, 84% of patients with an episode of "severe hypoglycemia" (defined as mood disorder hallucinations anafranil 10mg lowest price,40 mg/dL [2 depression symptoms forum best purchase anafranil. Despite recognition of hypoglycemia, 75% of patients did not have their dose of basal insulin changed before the next insulin administration (56). Studies of "bundled" preventative therapies including proactive surveillance of glycemic outliers and an interdisciplinary data-driven approach to glycemic management showed that hypoglycemic episodes in the hospital could be prevented. Compared with baseline, two such studies found that hypoglycemic events fell by 56% to 80% (57,58). The Joint Commission recommends that all hypoglycemic episodes be evaluated for a root care. Current nutrition recommendations advise individualization based on treatment goals, physiological parameters, and medication use. Consistent carbohydrate meal plans are preferred by many hospitals as they facilitate matching the prandial insulin dose to the amount of carbohydrate consumed (59). Regarding enteral nutritional therapy, diabetes-specific formulas appear to be superior to standard formulas in controlling postprandial glucose, A1C, and the insulin response (60). When the nutritional issues in the hospital are complex, a registered dietitian, knowledgeable and skilled in medical nutrition therapy, can serve as an individual inpatient team member. Orders should also indicate that the meal delivery and nutritional insulin coverage should be coordinated, as their variability often creates the possibility of hyperglycemic and hypoglycemic events. Glucocorticoid Therapy Diabetes self-management in the hospital may be appropriate for select youth and adult patients (61,62). Candidates include patients who successfully conduct self-management of diabetes at home, have the cognitive and physical skills needed to successfully self-administer insulin, and perform self-monitoring of blood glucose. If self-management is to be used, a protocol should include a requirement that the For patients receiving enteral or parenteral feedings who require insulin, insulin should be divided into basal, prandial, and correctional components. This is particularly important for people with type 1 diabetes to ensure that they continue to receive basal insulin even if the feedings are discontinued. Correctional insulin should also be administered subcutaneously every 6 h using human regular insulin or every 4 h using a rapid-acting insulin such as lispro, aspart, or glulisine. For patients receiving continuous peripheral or central parenteral nutrition, human regular insulin may be added to the solution, particularly if. A starting dose of 1 unit of human regular insulin for every 10 g dextrose has been recommended (65), to be adjusted daily in the solution. For full enteral/ parenteral feeding guidance, the reader Glucocorticoid type and duration of action must be considered in determining insulin treatment regimens. For long-acting glucocorticoids such as dexamethasone or multidose or continuous glucocorticoid use, long-acting insulin may be used (32,66). For higher doses of glucocorticoids, increasing doses of prandial and correctional insulin may be needed in addition to basal insulin (68). Perioperative Care Many standards for perioperative care lack a robust evidence base. Perform a preoperative risk assessment for patients at high risk for ischemic heart disease and those with autonomic neuropathy or renal failure. A recent study reported that, compared with the usual insulin dose, on average an approximate 25% reduction in the insulin dose given the evening before surgery was more likely to achieve perioperative blood glucose S178 Diabetes Care in the Hospital Diabetes Care Volume 42, Supplement 1, January 2019 levels in the target range with decreased risk for hypoglycemia (71). In noncardiac general surgery patients, basal insulin plus premeal short- or rapidacting insulin (basal-bolus) coverage has been associated with improved glycemic control and lower rates of perioperative complications compared with the traditional sliding scale regimen (short- or rapid-acting insulin coverage only with no basal insulin dosing) (38,72). Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State discharge, and its use is generally not recommended (80). For further information regarding treatment, refer to recent in-depth reviews (3). B A structured discharge plan tailored to the individual patient may reduce length of hospital stay and readmission rates and increase patient satisfaction (81). Discharge planning should begin at admission and be updated as patient needs change.