"Order proventil online from canada, asthma definition for dummies".
By: Y. Asam, MD
Clinical Director, University of Michigan Medical School
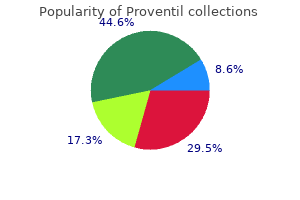
Other advantages of the laryngeal mask airway include its simplicity in learning and use asthma symptoms getting worse purchase cheap proventil on-line, fewer postoperative sore throats and coughing asthma 2014 movie trailer best purchase proventil, and less potential for laryngeal injuries asthma symptoms due to allergies purchase proventil 100 mcg with mastercard. These features also make the laryngeal mask airway an excellent instrument to use in many emergency situations involving the airway. Because this device can be inserted quickly and blindly, it has the potential to provide lifesaving ventilation while a more definitive airway is established. Since the laryngeal mask airway does not completely separate the airway from the esophagus, the greatest risk in using this device is pulmonary aspiration of regurgitated stomach contents. Contraindications to using this airway include patients with full stomachs or hiatal hernias, obesity, and emergency and abdominal surgeries. The need for controlled ventilation and prone or lateral positions are strong relative contraindications for elective use of this device. Understandably, if the mouth cannot be opened, the laryngeal mask airway is not useful. Other nonsurgical measures-Less common instruments and techniques used in difficult airway situations include the esophageal Combitube, light wand, and the Bullard laryngoscope. The esophagotracheal Combitube is an emergency airway management device for patients requiring rapid airway control. In many cases, this device can provide lifesaving emergency ventilation and oxygenation until a surgical airway can be established. Because of its design, the esophagotracheal Combitube can effectively ventilate the upper airway regardless of whether it is placed into the trachea or into the esophagus. If the Combitube tip is in the esophagus, ventilation is achieved through the proximal side ventilation holes of the esophageal port. If this device is inserted into the trachea during the blind intubation, ventilation is accomplished conventionally through the tracheal port. Because of its relatively large size, this Combitube is contraindicated in pediatric and very small adult patients. Finally, laryngospasm and laryngotracheal foreign bodies can impair ventilation if this device is inserted into the esophagus. The two basic surgical techniques to obtain an airway are cricothyroidotomy and tracheotomy. A tracheotomy is generally described as a procedure that involves opening the trachea. A tracheostomy is a procedure that exteriorizes the trachea to the cervical skin, resulting in a more permanent tracheal cutaneous fistula; therefore, the term tracheostomy should be reserved for these particular procedures. The indications for establishing an urgent surgical airway include the following: (1) severe maxillofacial trauma in which injuries make the airway inaccessible for translaryngeal intubation, (2) significant laryngeal trauma in which intubation may potentially cause more damage, (3) excessive hemorrhage or emesis obscuring landmarks required for successful intubation, (4) cervical spine injury with vocal cords that are difficult to visualize, and (5) failed translaryngeal intubation. In emergency situations, cricothyroidotomy is generally considered the pro- cedure of choice because it is fast and simple to perform and it requires very few instruments. It is technically more difficult, bloody, and dangerous compared with elective tracheotomy or cricothyroidotomy. There are rare circumstances in which an emergent tracheotomy is preferred over a cricothyroidotomy, such as true subglottic obstruction (eg, subglottic carcinoma or large thyroid tumors). Cricothyroidotomy should also be avoided in children because the cricoid cartilage is the narrowest portion of their airway. Tracheotomy-The primary objective of a tracheotomy is to provide a secure airway. The indications for performing a tracheotomy include (1) bypassing an upper airway obstruction, (2) providing a means for assisting mechanical ventilation (ie, chronic ventilator dependency), (3) enabling more efficient pulmonary hygiene, (4) temporarily securing an airway in patients undergoing major head and neck surgery, (5) relieving obstructive sleep apnea, and (6) eliminating pulmonary "dead space. Diagram of the neck, indicating locations of cricothyroidotomy and tracheotomy incisions. A tracheotomy is most easily performed if the patient is already intubated and general anesthesia has been administered.
Five-Finger Fern (Maidenhair Fern). Proventil.
- Are there safety concerns?
- What is Maidenhair Fern?
- How does Maidenhair Fern work?
- Bronchitis, coughs, whooping cough, menstrual problems, hair loss, promoting dark hair color, and others.
- Dosing considerations for Maidenhair Fern.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96557
If this treatment fails to asthma treatment europe cheap proventil 100mcg overnight delivery resolve the infection asthma definition trust generic proventil 100 mcg fast delivery, cortical mastoidectomy is indicated asthma definition symptoms order proventil cheap online. Intratemporal Complications Mastoiditis the fact that the mastoid air cell system is part of the middle ear cleft means that some degree of mastoid inflammation occurs whenever there is infection in the middle ear. Because of the close relationship of the ophthalmic division of the trigeminal nerve and the abducens nerve to the petrous apex, the classic features of petrositis are otorrhea associated with retroorbital pain and lateral rectus palsy (Gradenigo syndrome). Because of the high incidence of an intracranial extension of infection from petrositis, a combination of antibiotics and surgical drainage of the petrous apex is the management of choice. Intracranial Complications the incidence of intracranial complications has been considerably reduced since the introduction of antibiotics. Despite this fact, once an intracranial complication develops, it carries a significant risk to life. It is not uncommon for more than one intracranial complication to occur simultaneously. The most common early symptoms of intracranial extension of infection are persistent headache and fever. A decreasing level of consciousness and seizures are late signs associated with a poor prognosis. This situation should be managed by myringotomy with aspiration of pus from the middle ear along with antibiotic therapy, which will mostly result in the rapid resolution of paralysis. Further surgical exploration of the facial nerve is not indicated unless the paralysis fails to resolve. It can occur as a result of hematogenous spread, of direct extension from the middle ear through a bony dehiscence, or through the cochlear aqueduct via the inner ear. The most common organisms responsible for otic meningitis are S pneumoniae and H influenzae type B. The classic presentation is with headaches, photophobia, neck stiffness, and fluctuating levels of consciousness. Suppurative Labyrinthitis Infection of the middle ear can lead to direct bacterial invasion of the inner ear, usually via the round window, resulting in acute suppurative labyrinthitis. Erosion of the bony capsule of the inner ear by a cholesteatoma (most commonly the lateral semicircular canal) provides an alternative route of entry to the inner ear. Suppurative labyrinthitis presents with sudden sensorineural hearing loss, severe vertigo, nystagmus, and nausea and vomiting. The cochlear aqueduct provides a direct communication between the perilymph and the cerebrospinal fluid; therefore, there is a significant risk of developing meningitis. Surgical intervention is often required for underlying chronic middle ear disease, although the timing of surgery is controversial. Cochlear and vestibular functions are invariably permanently lost and, as healing occurs, obliterative osteitis of the inner ear commonly develops. Intracranial Abscess Brain, subdural, and extradural abscesses can all arise as a complication of middle ear infections (commonly associated with chronic disease). Intracranial abscesses are usually caused by multiple aerobic and anaerobic bacteria. Commonly cultured organisms include streptococci, S aureus, S pneumoniae, H influenzae, P aeruginosa, Bacteroides fragilis, and Proteus species. In addition to the generalized symptoms, focal neurologic signs can develop depending on the anatomic location of the abscess within the brain. As the abscess enlarges, features typical of raised intracranial pressure develop. Once a brain abscess has been diagnosed, urgent neurosurgical intervention is indicated to drain the abscess. Symptoms and signs tend to progress much more rapidly than those seen with a brain abscess. They can also occur in the posterior fossa, where they are commonly associated with lateral sinus thrombosis. The clinical features are often nonspecific and may fluctuate if a dehiscence in the tegmen is present, allowing the abscess to partially drain into the mastoid cavity.
With sophisticated ancillary tests and the accurate identification of localizing signs and symptoms asthmatic bronchitis june purchase 100mcg proventil overnight delivery, the surgical exploration of penetrating neck trauma is being used increasingly on a selective basis asthma symptoms night 100mcg proventil free shipping. Immediate operative exploration including triple endoscopy (direct laryngoscopy asthmatic bronchitis 3 month purchase proventil 100 mcg on line, bronchoscopy, and esophagoscopy) is used for all patients with hemodynamic instability or airway compromise. Injuries above the level of the arytenoids often heal spontaneously and may be expectantly managed. Lower hypopharyngeal and cervical esophageal injuries require open exploration, primary closure, and drainage due to the higher incidence of salivary leak, infection, and subsequent fistula. The stable patient is stratified depending on the presence of other signs or symptoms such as expanding hematoma, dysphonia, hemoptysis, hematemesis, or dysphagia. The first photograph (A) was taken before rigid fixation using a plating system; the second photograph (B) was taken after the plate was inserted. Note that the plate is carefully bent to restore the proper anterior commissure angle. Zone I injuries are studied with preoperative arteriography and often gastrograffin swallow studies because of the risk of occult injuries reported by some clinicians. With these patients, some evidence supports observation alone because the physical examination is extremely sensitive in detecting injuries that require operative intervention. In these patients, imaging and adjunctive testing are very helpful in guiding further management. Intubation injury-Intubation injuries may cause a wide variety of acute and chronic conditions. High endotracheal tube cuff pressures may cause progressive hoarseness or airway obstruction from glottic or subglottic edema. Compressive neuropathies caused by direct pressure of the cuff may lead to vocal fold paralysis. Mucosal injury is commonly seen, particularly in the posterior larynx and subglottis and usually results from pressure necrosis due to the presence of the tube and/or cuff or from traumatic intubation. These injuries may progress and lead to granuloma formation, fixation of the cricoarytenoid joint, web formation, or stenosis. The incidence of posterior glottic stenosis increases with the length of intubation and may occur in up to 14% of patients intubated for more than 10 days. Differentiating glottic stenosis from vocal fold paralysis can often be difficult, since both result in partial or complete vocal fold immobility. Most cases of granulation tissue formation seen after intubation trauma resolve spontaneously after some time. This treatment typically involves a combination of voice therapy and antireflux medication. This combination reduces the impact of behavioral and local inflammatory factors that are presumed to cause ongoing laryngeal irritation. In certain refractory cases, botulinum toxin injections can be used to forcibly reduce the impact of ongoing phonotrauma. Operative removal of the granuloma is rarely necessary except in cases of partial airway obstruction. It should be noted that surgical removal does not obviate the need for voice therapy and antireflux medications. Without controlling these factors, granulomas may recur after surgical excision alone. It may be detected weeks or months after extubation, when a patient presents for the evaluation of recent exercise intolerance or stridor. A keel may then be placed to prevent the web from reforming between apposed denuded mucosa. Posterior laryngeal stenosis and cricoarytenoid joint fixation are typically treated with repeated dilation through an endoscopic approach. However, occasionally, an open approach through a laryngofissure or the use of a stent is required.
The rash then usually spreads asthma symptoms 10 month old buy proventil overnight, especially to asthma symptoms for months purchase proventil overnight delivery exposed skin such as the arms and legs (Figure 45-5) asthma control definition order generic proventil pills, and then subsides over 1 to 2 weeks. B19 infection in adults causes polyarthritis (with or without a rash) that can last for weeks, months, or longer. The most serious complication of parvovirus infection is the aplastic crisis that occurs in patients with chronic hemolytic anemia. After 1 year of immunosuppressive therapy (mycophenolate mofetil, prednisone, and tacrolimus) after a kidney transplant, a 46-year-old man complained of dyspnea, lightheadedness, and fatigue upon exercise. Bone marrow analysis indicated erythroid hyperplasia with a predominance of immature erythroblasts. Proerythroblasts could be found, with deep basophilic cytoplasm and intranuclear inclusions that immunohistologically stained for B19 antigen. The patient received 16 units of packed red blood cells over 6 weeks, with continued anemia. Serology indicated the presence of IgM (1; 10) but insignificant IgG anti-B19 antibody. Immunosuppressive therapy of this patient prevented expansion and class switch to an IgG antibody response because of the lack of helper T cells. Resolution of the encapsidated parvovirus is dependent upon a robust antibody response, and in its absence, the normal transient anemia resulting from virus replication in erythroid precursors cannot be resolved. Box 45-5 Clinical Consequences of Parvovirus (B19) Infection Mild flulike illness (fever, headache, chills, myalgia, malaise) Erythema infectiosum (fifth disease) Aplastic crisis in persons with chronic anemia Arthropathy (polyarthritis: symptoms in many joints) Risk of fetal loss as a result of B19 virus crossing the placenta, causing anemia-related disease but not congenital anomalies Lytic infection phase Decreased reticulocyte and hemoglobin levels Virus in throat Viremia Noninfectious immunologic phase Virus-specific IgG antibody present Nonspecific flulike symptoms Incubation Fever, headache, chills, myalgia Rash/arthralgia (Erythema infectiosum) 28 people causes a transient reduction in erythropoiesis in the bone marrow. The reduction results in a transient reticulocytopenia that lasts 7 to 10 days and a decrease in hemoglobin level. An aplastic crisis is accompanied by fever and nonspecific symptoms such as malaise, myalgia, chills, and itching. The virus can infect the fetus and kill erythrocyte precursors, causing anemia, edema, hypoxia, and congestive heart failure (hydrops fetalis). Infection of seropositive pregnant women often has no adverse effect on the fetus. There is no evidence that B19 causes congenital abnormalities (Box 45-6; see Box 45-5). The more severe disease occurs in children younger than age 2, who may have bronchiolitis with wheezing and a viremia that extends long beyond the disease. The polymerase chain reaction test is a very sensitive method for detecting the B19 and bocavirus genomes in clinical samples. B19 causes biphasic disease: first, an initial lytic infection phase characterized by febrile flulike symptoms, and then a noninfectious immunologic phase characterized by a rash and arthralgia. Doe reported that her daughter had had a mild cold within the previous 2 weeks and that she herself was currently having more joint pain than usual and felt very tired. What underlying condition would put the daughter at increased risk for serious disease after B19 infection? The biphasic nature of the disease and the slapped-face rash are notable symptoms but are not unique to B19. A somewhat similar course of disease would occur with human herpesvirus 6 induction of exanthema subitum (roseola), although the time course may be different. The child was infectious during the initial disease signs and symptoms, which resemble a mild cold. The initial nonspecific disease signs are caused by interferon and other innate responses to the infection. The rash is caused by immune responses, most likely associated with antibody and virion immune complexes. The rash of the daughter and the arthralgia of the mother are due to the presence of antibody, formation of immune complexes, and type 2 and 3 hypersensitivity reactions. Pregnant women are at risk for B19 infection, which causes hydrops fetalis and loss of the fetus. Quarantine would not be effective because the virus is spread before the onset of the classic disease signs and symptoms of erythema infectiosum (fifth disease). The family has more than 230 members divided into nine genera, including Enterovirus, Rhinovirus, Hepatovirus (hepatitis A virus; discussed in Chapter 55), Cardiovirus, and Aphthovirus.