"Buy selegiline uk, treatment 4 pimples".
By: G. Jorn, M.A., M.D., M.P.H.
Clinical Director, Stanford University School of Medicine
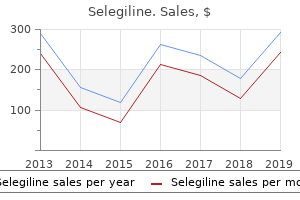
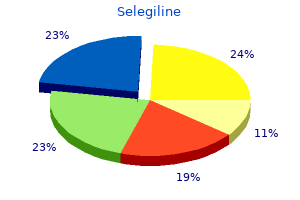
The renal mechanisms for potassium excretion adapt efficiently to symptoms genital herpes selegiline 5mg low price increases in the rate of potassium influx to treatment in statistics discount selegiline 5mg on line extracellular fluid symptoms xanax overdose generic selegiline 5mg without a prescription, particularly from dietary sources. Hence acute or chronic hyperkalemia due to exogenous potassium intake is uncommon, unless renal mechanisms for potassium excretion are compromised. In the latter setting, injudicious potassium administration may result in hyperkalemia. This occurs most commonly when intravenous potassium chloride is administered too rapidly, when potassium salts of antibiotics such as pencillin are administered, when transfusions are given with blood that has been stored for long periods, or when salt substitutes containing potassium are used. The occurrence of hyperkalemia in these settings usually requires that renal potassium excretion be impaired. Transcellular Shifts Acidosis beta-Adrenergic blockade Cell destruction Trauma, burns Rhabdomyolysis Hemolysis Tumor lysis Hyperkalemic periodic paralysis Diabetic hyperglycemia Insulin dependence plus aldosterone lack Depolarizing muscle paralysis Succinylcholine failure, however, either by the development of acidosis or, as indicated earlier, by the injudicious administration of potassium salts. This blockade of distal sodium absorption reduces luminal electronegativity and consequently impairs both proton secretion and potassium secretion. Thus, voltage-dependent renal tubular acidosis, like hyporeninemic hypoaldosteronism, is characterized by sodium wasting and hyperkalemia. In hyporeninemic hypoaldosteronism, the urine is acidic, and plasma levels of aldosterone are reduced even during volume contraction, whereas in voltage-dependent renal tubular acidosis there is impaired urinary acidification but a normal plasma aldosterone response to volume contraction. This shift occurs in acidosis or in circumstances that result in cell destruction; in the former, the serum potassium level rises by 0. Thus, the sudden occurrence of hyperkalemia in potassium-depleted patients is a diagnostic clue to the development of rhabdomyolysis. Hyperkalemic periodic paralysis is an autosomal dominant disorder in which sudden increases in the serum potassium level result in muscle paralysis. The hyperkalemia is often provoked by excessive dietary potassium intake or by exercise. Myotonia occurs commonly in the disorder and appears either between attacks or immediately preceding attacks. The acute paralytic attack can be treated by intravenous administration of calcium gluconate or glucose and insulin. Chronic treatment with diuretics such as acetazolamide minimizes the frequency of attacks. Paradoxical hyperkalemia occurs when sudden hyperglycemia develops in insulin-dependent diabetics who also have interstitial renal disease and associated hyporeninemic hypoaldosteronism. The insulin lack minimizes cellular re-entry of potassium, and the aldosterone deficiency blunts renal potassium excretion. The rise in plasma potassium concentration can be as high as 1 mEq/L in dialysis patients but usually is in the range of 0. Finally, anesthetic agents or other drugs that cause a depolarizing muscle paralysis, such as succinylcholine, promote potassium efflux from muscle cells. The loss of cell electronegativity in this situation increases passive potassium efflux from muscle cells. Essentially all patients on this drug combination increase their plasma potassium concentration within a few days of initiation of the therapy. The hyperkalemia is reversible with cessation of the drug and occurs as a consequence of inhibition of distal tubule potassium secretion. Pseudohyperkalemia may occur in thrombocytosis or leukocytosis, because clotting of blood promotes potassium release from these cells and may be identified by noting that the serum potassium level is elevated while the plasma potassium level is normal. The most important clinical manifestations of hyperkalemia relate to alterations in cardiac excitability. For this reason, the electrocardiogram is the single most important guide in appraising the threat posed by hyperkalemia and in determining how aggressive a therapeutic approach is necessary. The electrocardiographic manifestations of hyperkalemia, shown in Figure 102-8, follow directly from the effects of hyperkalemia on cardiac action potentials. The earliest manifestation of hyperkalemia is the development of peaked T waves, which become evident when the serum potassium level exceeds 6.
Repair of bile duct injuries is technically difficult medicine 503 order 5 mg selegiline with amex, and postsurgical strictures are associated with significant chronic morbidity medicine cabinet buy 5 mg selegiline visa, including biliary cirrhosis symptoms iron deficiency buy selegiline 5 mg otc. Chronic pancreatitis commonly produces fibrotic narrowing of the common bile duct where it passes through the head of the pancreas (see Chapter 141). Although proximal ductal dilatation and alkaline phosphatase elevation are common, significant cholestasis is unusual, and liver failure from biliary cirrhosis is quite uncommon. In patients with chronic pancreatitis who have elevations of serum alkaline phosphatase level or common bile duct dilatation on ultrasound examination, periodic liver biopsy has been recommended to detect progressive hepatic fibrosis. Surgical drainage (choledochojejunostomy) usually is successful in relieving ductal obstruction and halting the progression of biliary cirrhosis in chronic pancreatitis in the few cases in which it is required. Strictures of the bile ducts have been noted after hepatic irradiation, possibly secondary to vascular endothelial injury and ischemia. Similarly, strictures have been reported after chemotherapy employing intrahepatic arterial infusion of floxuridine or mitomycin C. Surgical drainage is preferred to endoscopic or percutaneous stenting in most patients with benign strictures because of uncertainties regarding long-term patency and late complications of stents. Liver flukes (see Chapter 432) are trematode parasites that are ingested in food, taken up from the gut, travel through the circulation to the liver, and from there pass into bile. The adult flukes mature in the biliary tree, where they can reside for decades and release eggs into bile. Mild infections usually are asymptomatic; heavier infections may produce fever and eosinophilia initially and later may cause signs and symptoms of biliary obstruction. Clonorchis sinensis and Opisthorchis viverrini are common in east Asia, where they are acquired through ingestion of raw fish. It is acquired from eating wild watercress on which encysted metacercariae have been deposited by snails. Liver flukes have been implicated in the pathogenesis of Oriental cholangiohepatitis, a chronic inflammatory disorder of the biliary tree associated with bile duct strictures, recurrent episodes of obstructive jaundice and ascending cholangitis, development of brown pigment gallstones in the intrahepatic and extrahepatic bile ducts, and biliary cirrhosis. This disorder is common in east Asia, including China and Japan, and is seen in the United States with some frequency in areas with large Asian immigrant populations. Not all patients have evidence of infection with liver flukes, and other pathogenic factors may be important. The disease is associated with lower socioeconomic class and malnutrition, and its frequency appears to have fallen dramatically in Japan, Hong Kong, and Taiwan 829 since the 1950s. Patients typically are younger than 50 years of age, with males and females affected equally. The usual presentation is an attack of ascending cholangitis associated with fever, right upper quadrant pain, and jaundice. Some attacks respond spontaneously or with antibiotic treatment alone; in others, sepsis may develop and surgical drainage may be required. Long-term management includes eradication of parasites and elimination of stones and strictures. Intrahepatic stones that cannot be extracted may necessitate resection of hepatic segments. The prognosis varies with the extent of involvement, but death from complications of sepsis and cirrhosis is common. Patients typically complain of right upper quadrant abdominal pain and often have abnormal liver test results, particularly that of alkaline phosphatase. Typically, the bile duct is normal at the time of birth; but over the next 6 to 12 weeks, its lumen gradually becomes obliterated and the duct becomes a fibrotic cord. Without treatment, over 90% of affected children will die before the age of 1 year from the complications of biliary cirrhosis. If the diagnosis is established promptly, a surgical portoenterostomy (Kasai procedure) can be of benefit. In this procedure, a core of tissue is removed from the hilum of the liver and the ends of the transected bile ducts are allowed to drain into a loop of jejunum. The Kasai procedure improves cholestasis and prolongs survival if performed early in infancy. Even after this procedure, most affected children progress to cirrhosis over the next few years. Biliary atresia is the most common indication for hepatic transplantation in young children.
Obliteration of the vasa recta compromises the operation of the medullary countercurrent system and impairs the ability to medicine for yeast infection buy selegiline 5 mg line generate and maintain medullary solute gradients useless id symptoms purchase selegiline 5mg fast delivery. A defect in urinary acidification is common and manifested as distal renal tubular acidosis with hyperkalemia and hyperchloremic metabolic acidosis (type 4 renal tubular acidosis) medications used to treat depression cheap selegiline online master card. Painless gross hematuria has been estimated to occur in up to 50% of patients with sickle cell nephropathy. Sickle cell "crisis," dehydration, hypoxemia, and the use of non-steroidal anti-inflammatory drugs predispose to papillary necrosis. Renal papillary necrosis is often "silent," but it may progress to chronic renal insufficiency and predispose the patient to repeated urinary tract infections. Nephrotic syndrome may occur in approximately 4% of patients with sickle glomerulopathy. Findings on renal biopsy usually indicate membranoproliferative glomerulopathy with segmental and global sclerosis. As this disorder progresses, glomerulopathy results in sclerosis and progressive loss of glomerular function, whereas papillary infarction can result in persistent hematuria. Volume depletion should be corrected by isotonic or hypotonic saline intravenously, as dictated by the serum sodium concentration. Hyperkalemia may require potassium exchange resin (sodium polystyrene, Kayexalate) per rectum or orally. When acidosis accompanies the hyperkalemia, alkali may help correct the hyperkalemia and the acidosis. Long-term administration of Shohl solution or sodium bicarbonate tablets may be necessary, and loop diuretics may be helpful. Potassium-sparing diuretics, non-steroidal anti-inflammatory drugs, or potassium supplements should be strictly avoided. Attempts to increase medullary blood flow and reduce medullary tonicity, including the use of distilled water, sodium bicarbonate, and diuretics such as mannitol or loop diuretics, may alleviate the hematuria. Rarely, small doses of epsilon-aminocaproic acid may be necessary for life-threatening hematuria but can result in thrombosis or ureteral obstruction. Unilateral or bilateral thrombosis of the major renal veins or their segments is a common but often subtle disorder that may develop in a variety of conditions. The serious risk for thromboembolic complications and vascular occlusion underscores the need for accurate and timely diagnosis and therapy. The reported incidence of renal vein thrombosis in patients with nephrotic syndrome is striking, ranging from 5 to 62%. Although some series emphasize a stronger association with membranous nephropathy, a prospective study of 26 patients with nephrotic syndrome demonstrated an association of renal vein thrombosis with a variety of glomerulopathies, including membranoproliferative, membranous, and proliferative glomerulonephritis and focal glomerular sclerosis. Renal vein thrombosis has also been reported in patients with sickle cell nephropathy, amyloidosis, diabetic nephropathy, renal vasculitis, and lupus nephritis, as well as allograft rejection. Circulating levels of proteins S and C may also be altered in nephrotic syndrome and contribute to the tendency toward thromboembolic complications. Renal vein thrombosis in infancy usually occurs in the setting of severe volume depletion and impaired renal blood flow. Extrinsic compression from retroperitoneal sources such as lymph nodes, retroperitoneal fibrosis, abscess, aortic aneurysm, or tumor may lead to renal vein thrombosis as a result of sluggish renal venous flow. Acute pancreatitis, trauma, and retroperitoneal surgery may also predispose to renal vein thrombosis. Renal cell carcinoma characteristically invades the renal vein and compromises venous flow, thereby resulting in renal vein thrombosis. The manifestations of renal vein thrombosis depend on the extent and rapidity of the development of renal venous occlusion. Patients with acute renal vein thrombosis may have nausea, vomiting, flank pain, leukocytosis, hematuria, renal function compromise, and an increase in renal size. Adult nephrotic patients with chronic renal vein thrombosis may have more subtle findings such as a dramatic increase in proteinuria or evidence of tubule dysfunction such as glycosuria, aminoaciduria, phosphaturia, and impaired urinary acidification.
The alarming symptoms of ethanol withdrawal are best managed by substituting another central nervous system depressant xerostomia medications side effects buy selegiline 5mg on line. However symptoms pinched nerve neck buy selegiline 5 mg lowest price, alcoholics undergoing withdrawal are very resistant to treatment genital warts selegiline 5mg overnight delivery sedatives (cross-tolerance), so large doses are often required to calm their agitation. Benzodiazepines are widely used to manage tremulousness and disordered perceptions during ethanol withdrawal. The goal is to suppress symptoms and produce mild sedation, and the drug dosage is adjusted to the severity of the withdrawal reaction. Treatment includes managing delirium and autonomic stability and preventing seizures. A sedative-hypnotic agent, typically a benzodiazepine, is prescribed as a substitute for alcohol, and the dose is tapered over several days. Patients with mild tremulousness and few associated symptoms usually respond to oral diazepam, 5 to 10 mg every 4 to 6 hours. The dosage is then reduced by 20 to 25% on successive days or increased if symptoms of ethanol withdrawal return. Detoxification can be carried out with close monitoring in an outpatient setting in socially stable patients with mild withdrawal. If withdrawal is more severe or accompanied by significant medical, surgical, or psychiatric illness or the patient is in an unstable social setting, inpatient detoxification may be needed. In such instances, benzodiazepines such as diazepam (Valium), chlordiazepoxide (Librium), oxazepam (Serax), or lorazepam (Ativan) are administered orally or parenterally in doses sufficient to keep the patient calm. Benzodiazepines should not be given intramuscularly because of inconsistent absorption. Patients may require hourly medication at doses that would be fatal in non-tolerant individuals. The first several days of severe alcohol withdrawal may require intravenous administration of total daily diazepam doses exceeding 400 mg (or the equivalent of other benzodiazepines) to achieve mild sedation. Multivitamin and thiamine supplementation should be continued, as should meticulous attention to electrolyte status. The benzodiazepine dosage can then be tapered by approximately 20 to 25% on successive days, with an increase in dosage if withdrawal symptoms recur. Once the symptoms of ethanol withdrawal are suppressed, it is necessary to avoid oversedation and the danger of respiratory depression by carefully titrating the dose of diazepam to just keep the patient calm. Alcohol withdrawal seizures can often be managed with intravenous benzodiazepines such as diazepam or lorazepam. Management of status epilepticus is the same as in other situations (see Chapter 484). Alcoholics are at increased risk for head trauma and central nervous system infection; studies to exclude these more serious diagnostic possibilities should be performed when seizures occurring in the setting of withdrawal display focal features or are accompanied by a prolonged post-ictal state or when status epilepticus intervenes. Long-term anticonvulsant therapy is not indicated for typical alcohol withdrawal seizures. Delirium tremens requires hospitalization and vigorous management in an intensive care setting. Mortality has reached 15% in the past, primarily because of injuries or associated medical disorders complicated by hyperthermia and dehydration. Volume depletion accompanying delirium tremens may cause circulatory collapse, and fluid losses can require replacement of 4 to 10 L in the first day. The goal of treatment is to control behavior and suppress symptoms without danger to the patient. Five to 10 mg or more of diazepam is given intravenously every 5 to 15 minutes until the patient is calm, and maintenance therapy is continued every 1 to 4 hours, as needed. Initially, as much as 200 mg of diazepam may be required before the agitation subsides. Seizures are unusual in patients with delirium tremens and should be evaluated promptly because of the possibility of meningitis or other disorders. Coexisting hepatic and cardiac disease may complicate fluid management, and the possibility that sedative agents may precipitate hepatic encephalopathy should be kept in mind. Alcoholics and alcohol abusers come to medical attention because of alcohol-related medical or psychiatric conditions, by referral from social service or criminal justice agencies, or through screening in clinical practice.
Transesophageal echocardiography is more accurate than transthoracic echocardiography in assessing endocarditis medications used to treat anxiety order selegiline 5 mg visa, particularly in regard to treatment west nile virus selegiline 5 mg sale complications and prosthetic valves medications 142 buy cheap selegiline 5mg line. Ischemic Heart Disease Disease of the coronary arteries is by far the most common cause of heart disease, and echocardiography is assuming an emerging role in assessing this disorder. Detection of regional dyssynergy is of value in identifying and sizing acute myocardial infarction (see Chapter 60). Furthermore, cardiac ultrasound is the modality of choice for assessing the complications of acute myocardial infarction such as ventricular septal defect, ruptured papillary muscle, pseudoaneurysm, and thrombi. Stress echocardiography has been shown to be superior to stress 194 Figure 43-1 Normal two-dimensional transthoracic echocardiogram in systole and diastole. A, With the transducer in the left parasternal location, images can be obtained parallel to the longitudinal axis of the left ventricle. This long-axis view depicts an elliptical left ventricle as visualized from the left shoulder, with the apex to the left and the base to the right. B, With the transducer in the left parasternal location, a perpendicular (short-axis) view of the left ventricle is obtained. C, Positioning the transducer at the apical impulse provides images of the perimeter of all four cardiac chambers and both the mitral and tricuspid valves (four-chamber view). The four-chamber apical view in systole is demonstrated with (left panel) and without (right panel) superimposed color Doppler flow imaging. A clear-cut mitral regurgitant jet can be seen emanating from a pre-acceleration area in the mitral orifice and penetrating backward into the left atrium (arrows). Documentation of enhanced contraction of hypokinetic or akinetic segments by cardiac ultrasound in response to low-dose inotropic stimulation with dobutamine is a good marker of viable myocardium, especially when high-dose stimulation induces recurrent contractile dysfunction. Cardiomyopathy Primary disease of the myocardium independent of other cardiovascular structures such as coronary arteries or valves (cardiomyopathy) has multiple causes, is often idiopathic, and is generally a diagnosis of exclusion. Echocardiography forms the cornerstone of the diagnostic strategy for cardiomyopathy (see Chapter 64). The approach aims first to classify the pathophysiology of the disorder as dilated (myocyte necrosis, profound dilation, and systolic dysfunction), hypertrophic (disproportionate septal thickening, obstructive or non-obstructive), or restrictive (generalized wall thickening with both systolic and diastolic impairment). Restrictive cardiomyopathy is characterized by generalized wall thickening, modest generalized hypokinesis, and evidence of impaired diastolic function. Causes associated with dilated myopathy include infection, inflammation, toxins, collagen vascular disease, and musculoskeletal disease. Hypertrophic cardiomyopathy is familial, whereas restrictive cardiomyopathy is associated with infiltrative processes such as amyloidosis and hemochromatosis. Echocardiography can establish and assess the severity of cardiomyopathy in nearly all cases, although cardiac catheterization or biopsy is occasionally necessary. Echocardiography plays a particularly important role in hypertrophic obstructive cardiomyopathy. Because asymmetrical septal hypertrophy and systolic anterior motion are fundamental manifestations of the disorder and are best detected by tomographic techniques, echocardiography is the modality of choice for diagnosis. The presence of mitral regurgitation and extent of hypertrophy can Figure 43-3 Dilated left ventricle with clot. An apical view of a four-chamber echocardiogram in a patient with dilated cardiomyopathy. The left ventricle is enlarged and spherical; a thrombus is seen at the cardiac apex (arrow). The parasternal long-axis view obtained in a patient with concentric hypertrophy due to systemic hypertension. The distance between calibration dots on the right is 10 mm so the wall thickness is 13 mm for both the septum and the posterior wall. In addition, echocardiography can detect dynamic subvalvular obstruction and quantify the gradient by virtue of the Bernoulli approach. Congenital Heart Diseases Congenital heart diseases represent fundamental distortions of cardiac anatomy (see Chapter 57).
5mg selegiline with visa. Alcohol Withdrawal Symptoms''Dizziness'' Alcoholism | Fear | Madness | Panic | Hallucination...