"Order generic ventolin line, asthma symptoms daily".
By: B. Aila, M.S., Ph.D.
Program Director, University of Wisconsin School of Medicine and Public Health
Gidal B asthma remission definition discount ventolin 100mcg line, Spencer N asthmatic bronchitis sleep buy discount ventolin online, Maly M asthma treatment emedicine ventolin 100 mcg with visa, Pitterle M, Williams E, Collins M, Jones J: Valproatemediated disturbances of hemostasis: relationship to dose and plasma concentration. Finsterer J, Pelzl G, Hess B: Severe, isolated thrombocytopenia under polytherapy with carbamazepine and valproate. Baltimore, Williams & Wilkins, 1993 [F] Treatment of Patients With Bipolar Disorder 71 Copyright 2010, American Psychiatric Association. Riva R, Albani F, Contin M, Baruzzi A: Pharmacokinetic interactions between antiepileptic drugs: clinical considerations. Tanaka E: Clinically significant pharmacokinetic drug interactions between antiepileptic drugs. Vasudev K, Goswami U, Kohli K: Carbamazepine and valproate monotherapy: feasibility, relative safety and efficacy, and therapeutic drug monitoring in manic disorder. Grossi E, Sacchetti E, Vita A: Anticonvulsants in affective disorders, in Carbamazepine Versus Chlorpromazine in Mania: A Double-Blind Trial. Okuma T, Inanaga K, Otsuki S, Sarai K, Takahashi R, Hazama H, Mori A, Watanabe M: Comparison of the antimanic efficacy of carbamazepine and chlorpromazine: a doubleblind controlled study. Dam M, Ekberg R, Loyning Y, Waltimo O, Jakobsen K: A double-blind study comparing oxcarbazepine and carbamazepine in patients with newly diagnosed, previously untreated epilepsy. Ichim L, Berk M, Brook S: Lamotrigine compared with lithium in mania: a double-blind randomized controlled trial. Arch Gen Psychiatry 2000; 57:841849 [A] Treatment of Patients With Bipolar Disorder 73 Copyright 2010, American Psychiatric Association. Leucht S, Pitschel-Walz G, Abraham D, Kissling W: Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo: a meta-analysis of randomized controlled trials. Sikdar S, Kulhara P, Avasthi A, Singh H: Combined chlorpromazine and electroconvulsive therapy in mania. Edwards R, Stephenson U, Flewett T: Clonazepam in acute mania: a double blind trial. Chouinard G: Clonazepam in acute and maintenance treatment of bipolar affective disorder. Meehan K, Zhang F, David S, Tohen M, Janicak P, Small J, Koch M, Rizk R, Walker D, Tran P, Breier A: A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating acutely agitated patients diagnosed with bipolar mania. Expert Opin Investig Drugs 2001; 10: 661671 [F] Treatment of Patients With Bipolar Disorder 75 Copyright 2010, American Psychiatric Association. Deveaugh-Geiss J, Ascher J, Brrok S, Cedrone J, Earl N, Emsley R, Frangou S, Huffman R: Safety and tolerability of lamotrigine in controlled monotherapy, in American College of Neuropsychopharmacology Annual Meeting Poster Abstracts. Smeraldi E, Benedetti F, Barbini B, Campori E, Colombo C: Sustained antidepressant effect of sleep deprivation combined with pindolol in bipolar depression: a placebo-controlled trial. Colombo C, Lucca A, Benedetti F, Barbini B, Campori E, Smeraldi E: Total sleep deprivation combined with lithium and light therapy in the treatment of bipolar depression: replication of main effects and interaction. Peet M: Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Okuma T, Inanaga K, Otsuki S, Sarai K, Takahashi R, Hazama H, Mori A, Watanabe S: A preliminary double-blind study on the efficacy of carbamazepine in prophylaxis of manicdepressive illness. Maj M, Pirozzi R, Magliano L, Bartoli L: Long-term outcome of lithium prophylaxis in bipolar disorder: a 5-year prospective study of 402 patients at a lithium clinic. Biol Psychiatry 1999; 45:953958 [G] Treatment of Patients With Bipolar Disorder 77 Copyright 2010, American Psychiatric Association. Coryell W, Winokur G, Solomon D, Shea T, Leon A, Keller M: Lithium and recurrence in a long-term follow-up of bipolar affective disorder. Greil W, Kleindienst N, Erazo N, Muller-Oerlinghausen B: Differential response to lithium and carbamazepine in the prophylaxis of bipolar disorder. Godemann F, Hellweg R: [20 years unsuccessful prevention of bipolar affective psychosis recurrence. Psychiatr Serv 1998; 49:531 533 [A] Treatment of Patients With Bipolar Disorder 79 Copyright 2010, American Psychiatric Association. Colom F, Vieta E, Benabarre A, Martinez-Aran A, Reinares M, Corbella B, Gasto C: Topiramate abuse in a bipolar patient with an eating disorder. Watanabe S, Ishino H, Otsuki S: Double-blind comparison of lithium carbonate and imipramine in treatment of depression. Hassanyeh F, Davison K: Bipolar affective psychosis with onset before age 16 years: report of 10 cases. Strober M, DeAntonio M, Schmidt-Lackner S, Freeman R, Lampert C, Diamond J: Early childhood attention deficit hyperactivity disorder predicts poorer response to acute lithium therapy in adolescent mania.
Additional information:
Potential the Health Benefits of Smoking Cessation 195 A Report of the Surgeon General Table 4 asthma symptoms in child cheap 100 mcg ventolin. The Health Benefits of Smoking Cessation 197 A Report of the Surgeon General Table 4 asthma definition 7 stages cheap 100mcg ventolin free shipping. The Health Benefits of Smoking Cessation 199 A Report of the Surgeon General Table 4 asthma treatment with exercise buy cheap ventolin 100 mcg on line. This meta-analysis also pooled data that included information on number of years since cessation from three case-control studies (Severson et al. Results of studies published since 1990 expand the role of smoking as a cause of cancer and support the reduction of cancer risk following smoking cessation. The 12 types of cancer reviewed in this section have all been judged to be caused by cigarette smoking in reports of the U. Because smoking cessation reduces cumulative exposure to tobacco smoke across the life course, biological plausibility alone, coupled with appropriate temporality, supports the conclusion that smoking cessation reduces the risk of all 12 cancers that have been causally linked to cigarette smoking. Additionally, epidemiological evidence documents that the risk for most of these cancers drops progressively as the time since successful quitting lengthens, and findings are generally consistent across studies. The effect of smoking cessation on risk for lung cancer is particularly important because lung cancer is the largest contributor to smoking-attributable cancer mortality in the United States and the number of new cases continues to increase (U. Since 1990, many studies have been published characterizing how risk for lung cancer changes with time since smoking cessation. Taken together, these epidemiological findings support a causal association between smoking cessation and lower risk for liver cancer. Taken together, these epidemiological findings, including those of incident colorectal cancer and established precursor lesions for colorectal cancer, support a causal association between smoking cessation and lower risk for colorectal cancer. The evidence is sufficient to infer that smoking cessation reduces the risk of kidney cancer. The evidence is sufficient to infer that smoking cessation reduces the risk of laryngeal cancer. The evidence is sufficient to infer that smoking cessation reduces the risk of cancers of the oral cavity and pharynx 4. The evidence is sufficient to infer that smoking cessation reduces the risk of esophageal cancer. The evidence is sufficient to infer that smoking cessation reduces the risk of pancreatic cancer. Implications the evidence that smoking cessation reduces cancer risk has long been an important part of the rationale for efforts-including educational, clinical, health systems, community, and population-based interventions and initiatives to make evidence-based, barrier-free cessation services widely available-to motivate and help smokers to quit. Smoking Cessation After a Cancer Diagnosis this section reviews evidence of the health benefits of smoking cessation at the time of a cancer diagnosis or after that diagnosis compared with continuing to smoke. At the time of cancer diagnosis, approximately 2030% of all cancer patients self-reported current cigarette smoking (Warren and Simmons 2018); however, self-reported rates of smoking were typically lower than biochemically confirmed smoking, as smokers with cancer may misrepresent their smoking. Among long-term cancer survivors, the smoking prevalence is approximately 9% (Warren and Simmons 2018). This review is limited to all-cause mortality, an integrative indicator, and does not explore disease progression or recurrence, cancer-specific mortality, second primary cancer, quality of life, or treatment toxicity as outcomes of interest. The 2014 report was also the first to conclude that continued smoking after a cancer diagnosis causes adverse health outcomes among cancer patients or survivors. Studies were excluded if they reported findings on only continued smoking after a cancer diagnosis versus quitting smoking substantially before a cancer diagnosis. The cohorts were composed of patients with lung cancer (four studies), with head/neck cancer (three studies), with breast cancer (one study), and with multiple types of cancer (two studies). Eight studies did not specify the treatment modality (surgery, radiotherapy, chemotherapy), and two patient cohorts were composed exclusively of patients treated with radiotherapy (Al-Mamgani et al. In all three studies, continued smoking after a cancer diagnosis significantly increased risk of mortality compared with never smoking, and the risk of mortality for quitters was greater than that for never smokers but not as great as that for continuing smokers. Four studies compared continued cigarette smoking with quitting, using quitters as the referent (Tao et al. In all four studies, continued smoking was associated with increased all-cause mortality relative to quitting. For a group of 1,632 male cancer patients from the Shanghai Cancer Cohort (Tao et al. Smoking Cessation and All-Cause Mortality in Cancer Patients Ten studies (seven prospective cohort studies and three retrospective cohort studies) reporting on 10,975 patients met the inclusion criteria (Table 4. The Evaluation of the Evidence this is the first review in a report of the Surgeon General on the potential health benefits of smoking cessation after a cancer diagnosis.
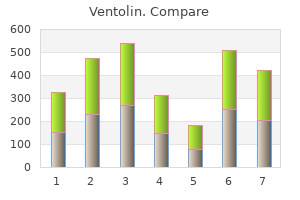
However asthma breathing exercises order ventolin cheap, an evaluation of multiple interventions should be based on incremental cost-effectiveness ratios asthma definition 90937 discount 100 mcg ventolin with mastercard. Relying only on absolute cost-effectiveness ratios can distort estimates and result in invalid conclusions asthma symptoms 8 months best 100 mcg ventolin. The absolute cost-effectiveness ratios of alternative interventions can be similar and cost-effective when compared with an acceptable threshold. However, when the incremental cost-effectiveness ratio for an alternative is evaluated and compared with the next best alternative, the alternative may not necessarily be cost-effective- even if it is cost-effective when compared with the control. An international consortium that evaluated the relative costs and benefits of a range of smoking cessation interventions found that in a high-income country, such as the United States, such interventions as automated text messaging, self-help materials, and brief advice from a physician have a low cost but only small effects on smoking cessation. Conversely, pharmacological and psychological interventions (either by telephone or provided in person) are higher in cost but have greater effects on increasing smoking cessation (West et al. A systematic review on the economic impact of a conservative 20% price increase of tobacco products through taxation found evidence of per capita cost savings over the short- and medium terms (Contreary et al. Because of their relatively high cost, pharmacologic and psychologic smoking cessation interventions have been more closely evaluated than inexpensive interventions. This report summarizes the cost-effectiveness ratios gleaned from the review of literature on the costeffectiveness of clinical cessation interventions and compares the estimates to a threshold of cost-effectiveness for clinical interventions used in healthcare (Neumann et al. Cost-Effectiveness of Clinical Smoking Cessation Interventions In a systematic review of the literature, Ruger and Lazar (2012) summarized the evidence on the costeffectiveness of smoking cessation through 2009. To standardize dollar value of costs to the same base year, estimates in this section were converted to 2017 U. Among two studies on pharmacistdirected smoking cessation programs, one involving only the receipt of advice and motivation compared with usual advice from a pharmacist found cost-effectiveness ratios ranging from $628 to $2,678 per life-year saved from the payer perspective (Crealey et al. Incremental cost-effectiveness ratios ranged from $1,409 to $5,838 per quit attempt from the healthcare system perspective (Hoogendoorn et al. One study compared bupropion with counseling or advice alone and found that the incremental cost per life-year saved ranged from $1,603 to $3,746 from a national health system perspective (Song et al. The Benefits of Smoking Cessation on Overall Morbidity, Mortality, and Economic Costs 473 A Report of the Surgeon General Table 5. The Benefits of Smoking Cessation on Overall Morbidity, Mortality, and Economic Costs 477 A Report of the Surgeon General Table 5. The Benefits of Smoking Cessation on Overall Morbidity, Mortality, and Economic Costs 481 A Report of the Surgeon General that incremental cost-effectiveness ratios ranged from $3,809 to $16,769 per life-year saved compared with usual care from the implementing hospital perspective (Meenan et al. Three evaluations of counseling therapies per additional quit found that the incremental cost-effectiveness ratio was $8,382 from the implementing hospital perspective (Meenan et al. In other studies that compared brief counseling or smoking cessation programs with usual care, estimated incremental cost-effectiveness ratios ranged from $499 to $1,875 per life-year saved from the school perspective (Dino et al. To standardize the dollar value of costs to the same base year, estimates in this section were converted to 2017 U. Although these studies share this focus, the evaluations were highly heterogeneous (Ekpu and Brown 2015). Regardless, some of these evaluations estimated cost-effectiveness ratios similar to or greater than those for clinical smoking cessation interventions. Synthesis of the Evidence the evidence on cost-effectiveness of smoking cessation and the resulting reduction in healthcare expenditures as a result of cessation strongly indicate that smoking cessation interventions should be implemented throughout the healthcare system and supported more broadly by population-level tobacco control measures. The selection of the intervention depends on the feasibility of the intervention and on the context of an organization and its ability to fund the intervention. Current estimates of the cost-effectiveness of smoking cessation are limited by the variation in methodologies, including heterogeneity in comparators and perspectives. Despite specific recommendations made two decades ago to enhance the comparability of economic evaluations (Gold et al. Estimates converted to 2017 dollars from the base case year (or publication year if no base case year) using the Medical Care part of the Consumer Price Index (all urban consumers). The new recommendations from the second Panel on Cost-Effectiveness in Health and Medicine, which were published after the publication of many of the studies reviewed in this chapter, emphasize the need for compliance with the recommendations for consistency and comparability of studies (Sanders et al. Additionally, current trends in cigarette smoking and other forms of tobacco product use affect estimates of economic expenditures from smoking and smoking cessation. Nonetheless, the scientific evidence clearly documents that smoking cessation interventions reduce smoking-attributable expenditures.